ACAP Member Health Plans Tackle Large-Scale Re-Enrollment & Health Equity Priorities
Re-enrollment and social health equity are the focal points of community health plans across the United States as they tackle important hurdles to health for millions of the nation’s patients. With the end of the Public Health Emergency (PHE) looming on July 15th, even with a potential extension to October, Medicaid members could see a gap in coverage, upwards of 15 million individuals, according to the Association of Community Affiliated Plans (ACAP). As we know, Health and Human Services declared COVID-19 a PHE in January of 2022. With Congress passing the Families First Coronavirus Response Act (FFCRA) in March of 2020, states were prohibited from terminating Medicaid coverage during the PHE, therefore reducing churn in coverage for patients during that time. According to Centers for Medicare & Medicaid Services (CMS), “The expiration of the continuous coverage requirement authorized by the Families First Coronavirus Response Act (FFCRA) presents the single largest health coverage transition event since the first open enrollment period of the Affordable Care Act.”

Significant resourcing is underway by states to fill the need for re-enrollment when the continuous enrollment period ends. Though CMS and states are partnering with Medicaid health plans to minimize disruptions in coverage, there are numerous hurdles that the plans are facing depending on statewide regulations, including, the disallowing of health professionals to aid in patient sign-ups or the need for a patient to provide a signature on the form – limiting a phone or digital sign up for many. Each state across the United States has a significant risk of seeing individuals have a gap in coverage. According to the Kaiser Family Foundation (KFF), of 43 states who responded, there are four categories of approaches on how states will approach prioritizing renewals and pending actions at the end of the continuous enrollment: 1. Population-based approach; 2. Time-based approach; 3. Hybrid approach; and 4. To be determined. CMS guidance gives states “up to 12 months to initiate and 14 months to complete the backlog of redeterminations,” according to KFF. So, it will be a year before most states return to routine operations.
In addition to the work health plans are doing to support re-enrollment, advances continue to be made in the health equity programs offered to members. These social service resources range from food delivery and food preparation training, to transit, housing, and much more.
CMS supports health equity efforts to address the health disparities in the nation’s health system and in order to achieve quality, person-centered, affordable care, according to Dr. Meena Seshamani, Deputy Administrator & Director, Centers for Medicare & Medicaid Services. To do so, she added at a recent meeting for ACAP, Medicare is improving operations to better measure and target disparities through improved data collection and analysis, as well as new metrics to assess the ways in which providers make operational changes. Further, CMS - with stakeholder partnership engagement - is “infusing health equity into Medicare payment incentive programs, increasing access to behavioral health services, and funding new medical residency positions in hospitals serving rural and underserved communities.”
With more than 12 million Americans dual-eligible (qualifying for both Medicare and Medicaid), these commitments will be necessities. A number of plans have joined ACAP’s Health Equity Learning Collaborative to listen and learn, measure and improve, and to create policy around improving health equity. To share best practices in the field of Social Determinants of Health, ACAP launched SDOH Innovation. The organization will offer tools and resources for policymakers, thought leaders, and others in the healthcare ecosystem – all to cultivate work being done to support health equity. Learn more at https://sdohinnovation.org/

Where does Nokomis fit into all of this?
As a partner in ensuring claim accountability, Nokomis provides PMPM monthly dollar savings for these plans so that they can then use those dollars for programs supporting health equity – not paying inaccurate claims. Nokomis genuinely cares about the entire healthcare ecosystem, and understands that the claims system plays a critical role.
Unlike other companies, Nokomis does not decide which claims to review by dollar amount and has no minimum claim amount. Instead, Nokomis focuses on multiple points of review before requesting medical records. All completed reviews are supported by external requirements, guidelines, and rules to find claim inaccuracies. Nokomis calls this holistic approach “Claim Accountability,” which aims not to be a punitive system, but to increase accountability, honesty, and accuracy in healthcare claim submissions using a combination of technology and human review.
In light of the challenges community plans are facing, they do not need inaccurate claims tying up their dollars—for example, being charged $2,750 for just a urine cup as part of a routine urine test, when those dollars can be spent to provide social health services to some of the most vulnerable patients.
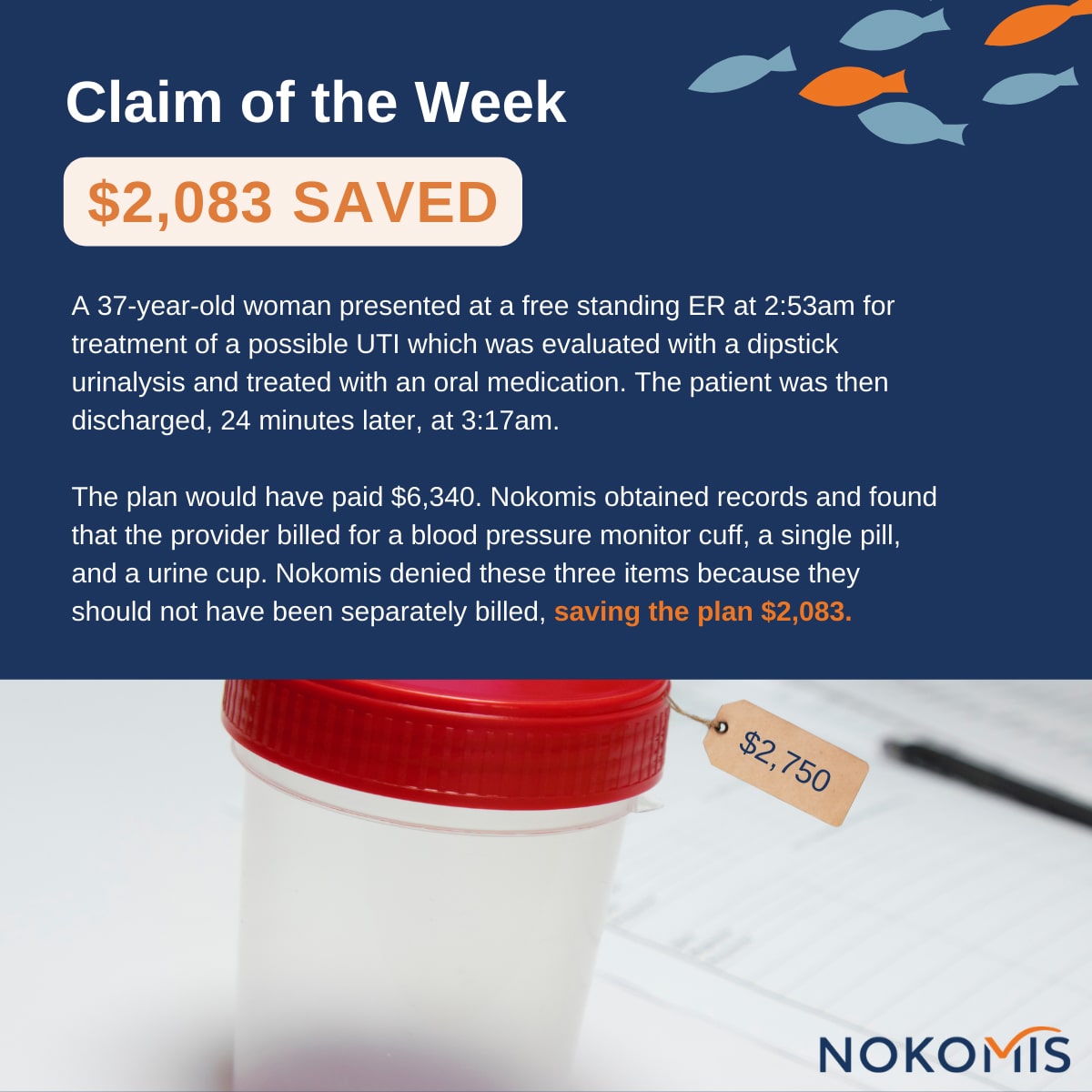
Nokomis helps plans understand where claim inaccuracies are happening, before payment, allowing plans to divert these savings towards member-focused programs. Moreover, with time and training workshops, Nokomis helps providers improve their claim accuracy rates –– usually saving an average of 9% on top of any additional payment integrity systems they might already have in place –– which not only builds a more equitable and accurate claim system, but frees up additional funds for programming.
Nokomis recognizes the importance of low patient and provider relationship friction and provides a customized approach to all communications around claim accountability.
Learn more about the impact Nokomis can have for a plan by emailing info@nokomishealth.com.