Studies have shown that up to 80% of medical claims are submitted with errors.
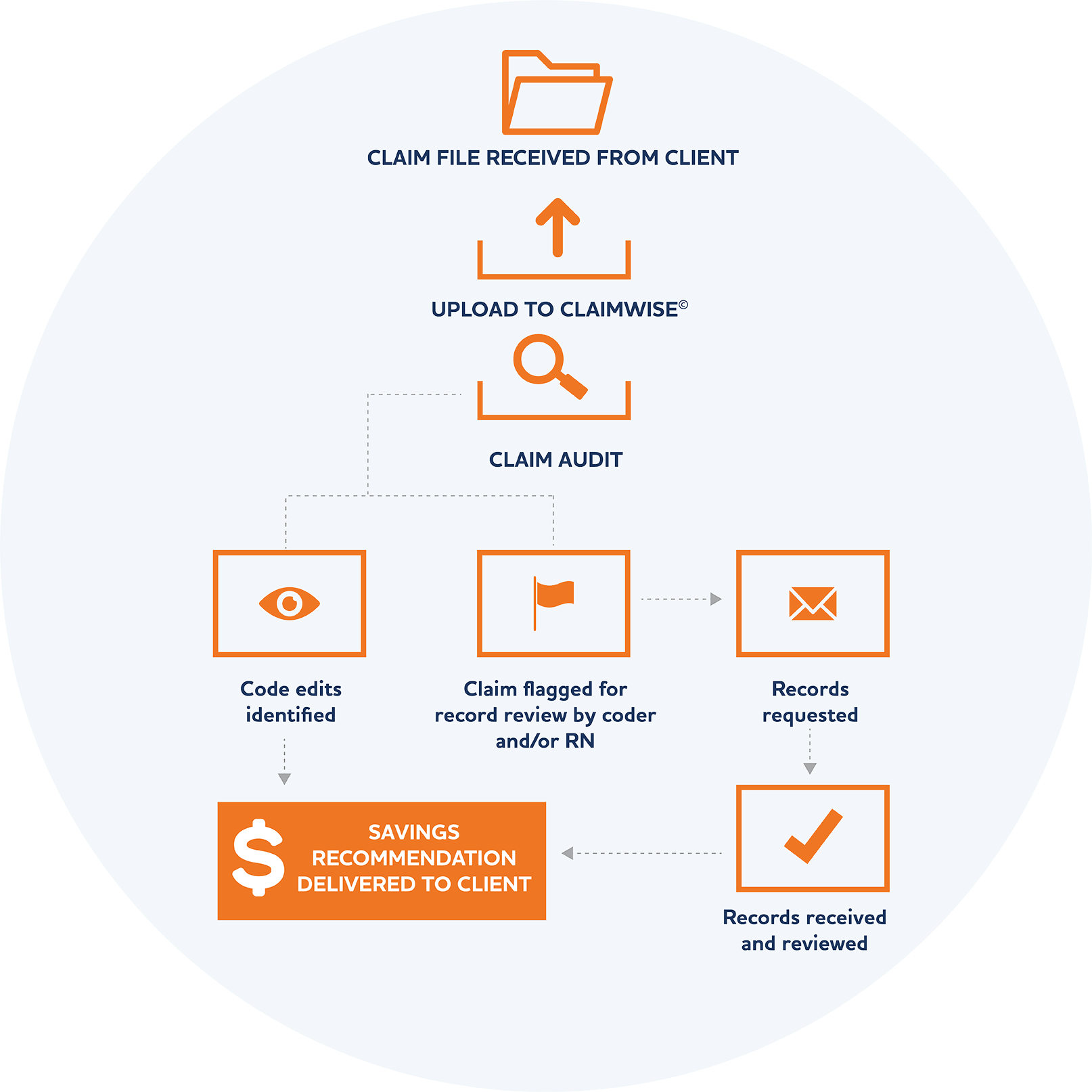
For many payors, it is difficult enough to just get the claim paid correctly, let alone to review the claim more deeply for billing and coding errors. Many code editing systems and bill review vendors are unable to provide a comprehensive solution to identify billing errors. At Nokomis, we are equipped to dig deeper, provide more sophisticated edits, and perform faster via our ClaimWiseTM review engine.
Innovation & Human Expertise
Our extensive industry knowledge and years of experience informed the need to develop our own proprietary claim review engine, ClaimWiseTM. Rather than working with an off the shelf system and trying to customize it to meet our clients’ needs, we built ClaimWiseTM from the ground up using APEX software and a team of expert developers. Powered by Oracle, ClaimWiseTM allows for rapid review of medical claims.
Claims are passed through hundreds of custom-built rules, millions of code edit combinations, and scores of reference tables. We know the importance of timely processing and with ClaimWiseTM we are equipped to return 100% of concurrent claims to our clients within one business day.

Our system is designed to function as a fully customizable dial.
Demand Based & Fully Customizable
ClaimWiseTM is fully customizable to our clients’ needs. We can turn rules and edits on or off for a particular client and we can customize our business rules to make claim edits more or less aggressive, depending on the client’s needs and requirements.
Seamless Integration & Hassle-Free Implementation
We know that our clients are busy, so we make the implementation process as painless as possible. We do the “heavy lifting” wherever we can, including adapting our file layouts to our clients’ format for seamless integration. We can accommodate both 837 and flat files. We lead our clients step-by-step throughout the entire process, resulting in a straightforward, transparent, hassle-free implementation.
ClaimWiseTM Case Studies
A 44 year old female received radiation therapy for treatment of metastatic breast cancer. Nokomis obtained records to confirm the procedure codes that were billed and found numerous errors on the claims. Savings were $12,600 on total charges of $21,000.
A 27 year old male was treated in the emergency department for a laceration to his leg. The client was ready to pay the claim but we investigated the cause of the accident and found that the member was injured at his work site, so the claim was denied and referred to the workers comp carrier for payment. This resulted in savings of over $9,000 to the plan.
Nokomis’s ClaimWiseTM rules engine identified a surgeon claim for a member who had no other claims for that date of service. We interviewed the patient and requested records and determined that the bill was sent in error. We denied the claim, resulting in savings of $8,200.