ClaimWise™: A deeper look at Nokomis’ powerful claim review engine
Part of the founding story at Nokomis was our CEO, Rich Henriksen, identifying the need for both a more accurate claim review engine, and a stronger team of expert reviewers to use that engine. After spending 35+ years in healthcare on both the plan & provider sides of the business, Rich built a team to do just that.
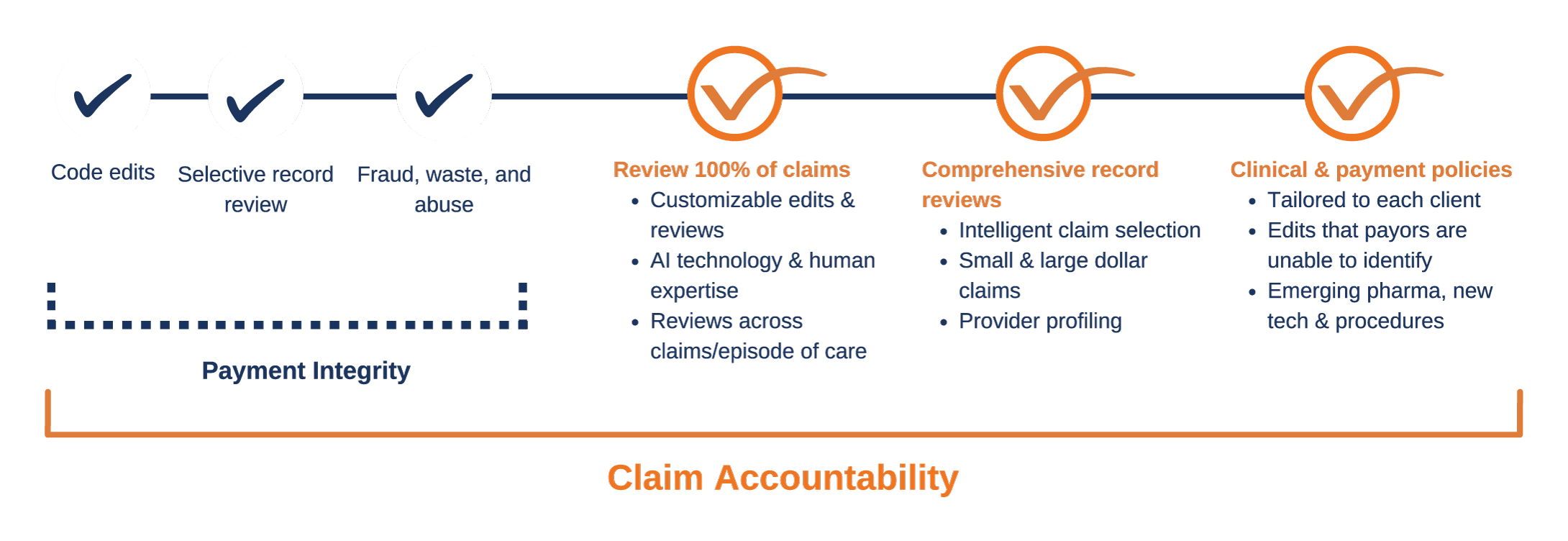
Part of that equation was the creation of Nokomis’s ClaimWise™ technology, which we’ll dive into here. That said, we want to make it explicit that, at Nokomis, while ClaimWise™ is a powerful part of our claim review process, the work we do wouldn’t be possible without our team of expert reviewers & analysts. All of our team members have worked across the healthcare ecosystem and have been reviewing claims on both the provider and plan sides for decades. Combining human expertise and technological innovation gives us a truly holistic and unique perspective when it comes to ensuring accurate claims. We’ve coined this approach “Claim Accountability.”
We developed our own proprietary claim review technology, ClaimWise™, rather than working with an off-the-shelf system because we recognized the need to customize technology for health plans’ specific needs and relationships. Powered by Oracle, the Nokomis team built ClaimWise™ from the ground up using APEX software and a team of expert developers. Our team of developers are incredibly skilled in APEX, which allows us to develop and accommodate customizations that other systems may not be able to handle.
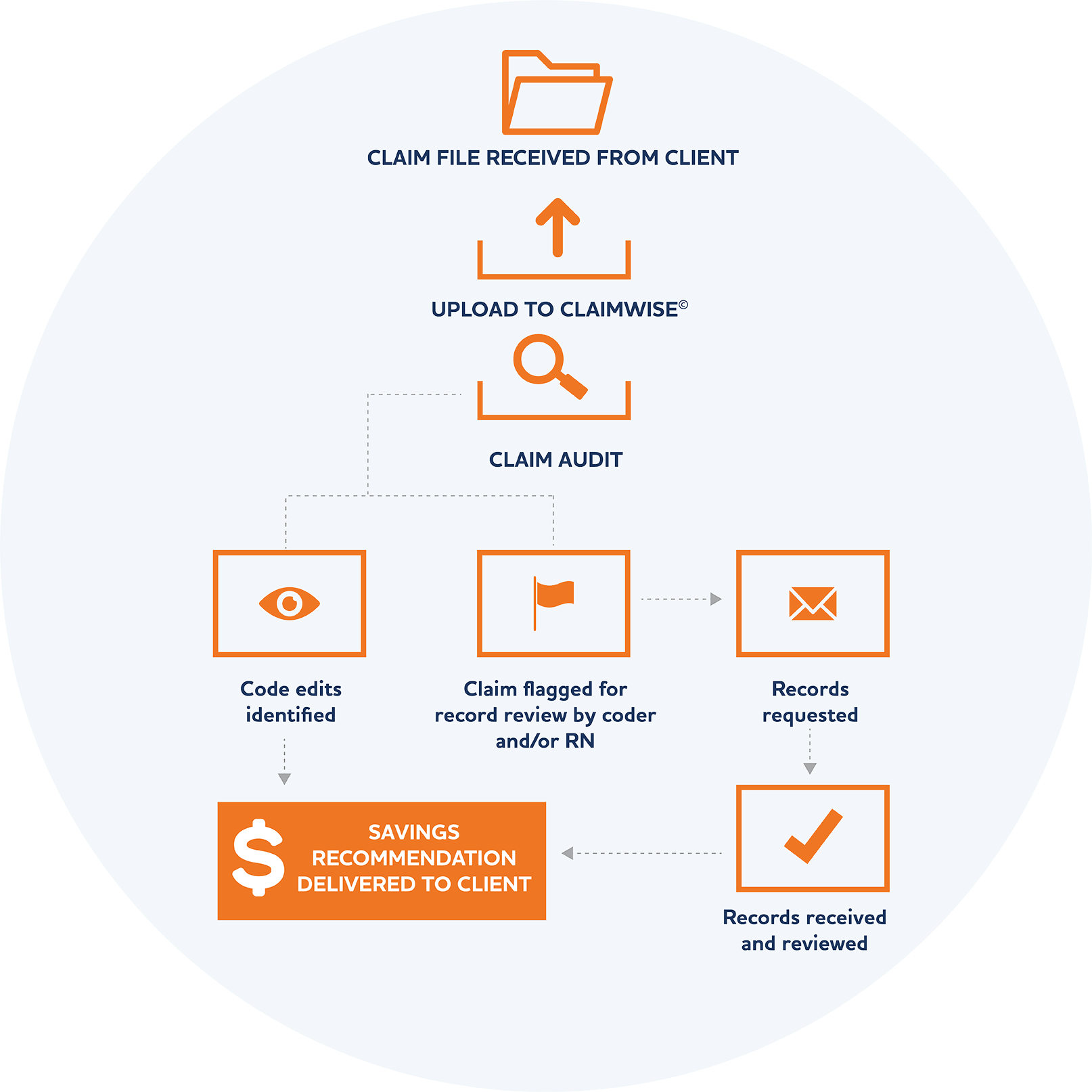
When a claim is submitted to ClaimWise™, it’s passed through hundreds of custom-built rules, millions of code edit combinations, and scores of reference tables. This process uses intelligent claim selection to identify claims that likely contain inaccuracies, which our team of expert coders, reviewers, and analysts will then further investigate and request records as needed. Because this process is so efficient, we’re equipped to return 100% of concurrent claims to our clients within one business day, but often within minutes or hours. Since ClaimWise™ is fully customizable to our clients’ needs, we can turn rules and edits on or off for a particular client, and we can customize business rules to make claim edits more or less aggressive depending on client requirements.
Since our entire team has worked with providers, health systems, health plans, and more, we worked to ensure that ClaimWise™ was not only accurate and customizable, but as easy to implement as possible. Of course adding any new system will come with a brief learning curve, but our team is dedicated to supporting our clients and their members at every step. We’ll always do the “heavy lifting” wherever we can, from adapting our file layouts to our clients’ format, to directly handling any rare balance-billing issues that may arise (although 99.3% of our recommendations see no appeals). Additionally, we designed ClaimWise™ to work alongside any existing systems already in place for payment integrity–we generally still save our clients on average an additional 9% on top of whatever savings their other systems may be identifying.

One of the reasons ClaimWise™ assists us in saving that additional 9% that other systems overlook is that we’re experts at finding inaccuracies in claims that look “okay” at face value. The only way to know for sure what happened in an exam room is to request records, and we do request records when needed. Additionally, we run all claim submissions through ClaimWise™ regardless of dollar amount or provider type—trust us, the small dollar savings really add up.
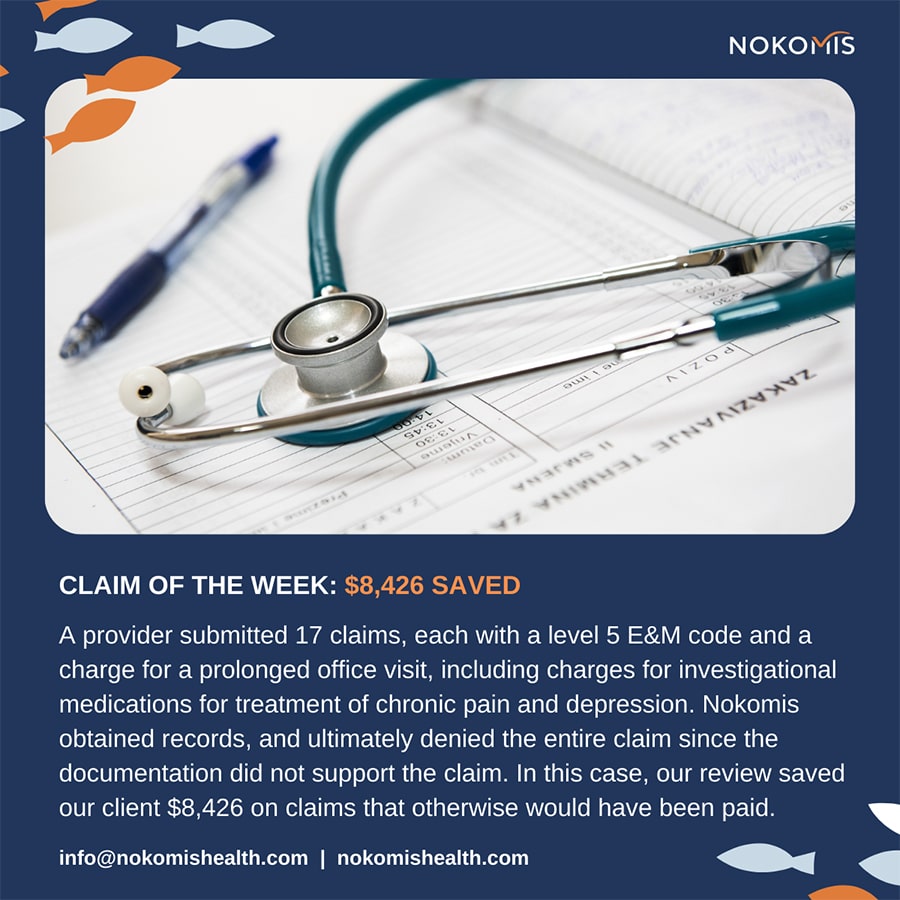
Check out some of the claim savings examples below, and follow us on LinkedIn so you never miss out on one of our “Claim of the Week” highlights:

At Nokomis, our ultimate mission is to improve accountability in healthcare claim submissions and a huge part of what makes that mission possible is ClaimWise™. Paired with our incredible team of coders, ClaimWise™ allows us to independently review claims:
- that might look okay at face value
- regardless of dollar amount
- before payment
- in one business day