This is our key differentiator; doing both processes together sequentially over every single claim, irrespective of value uncovers claims that you should not be paying that no else finds.
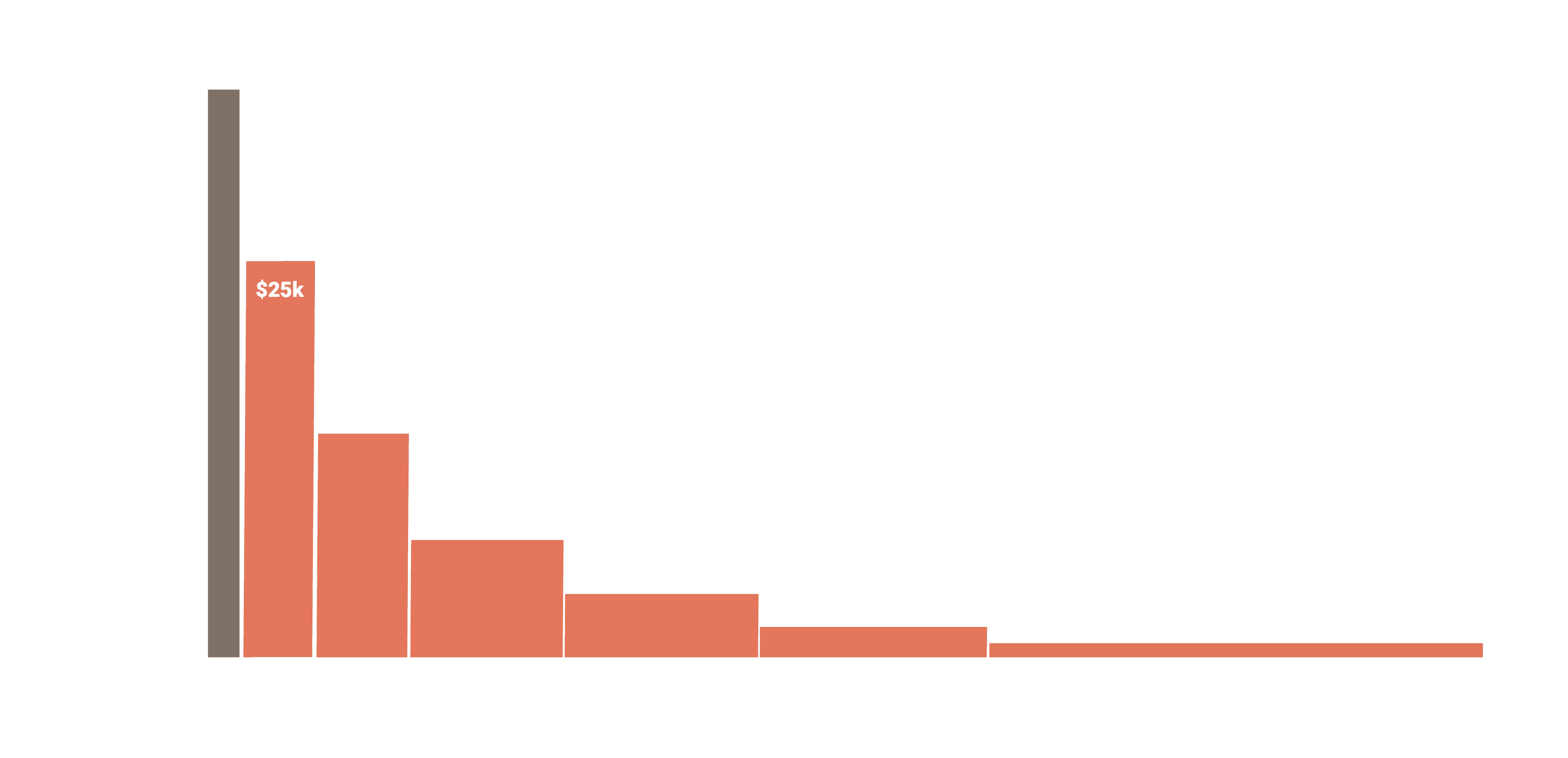
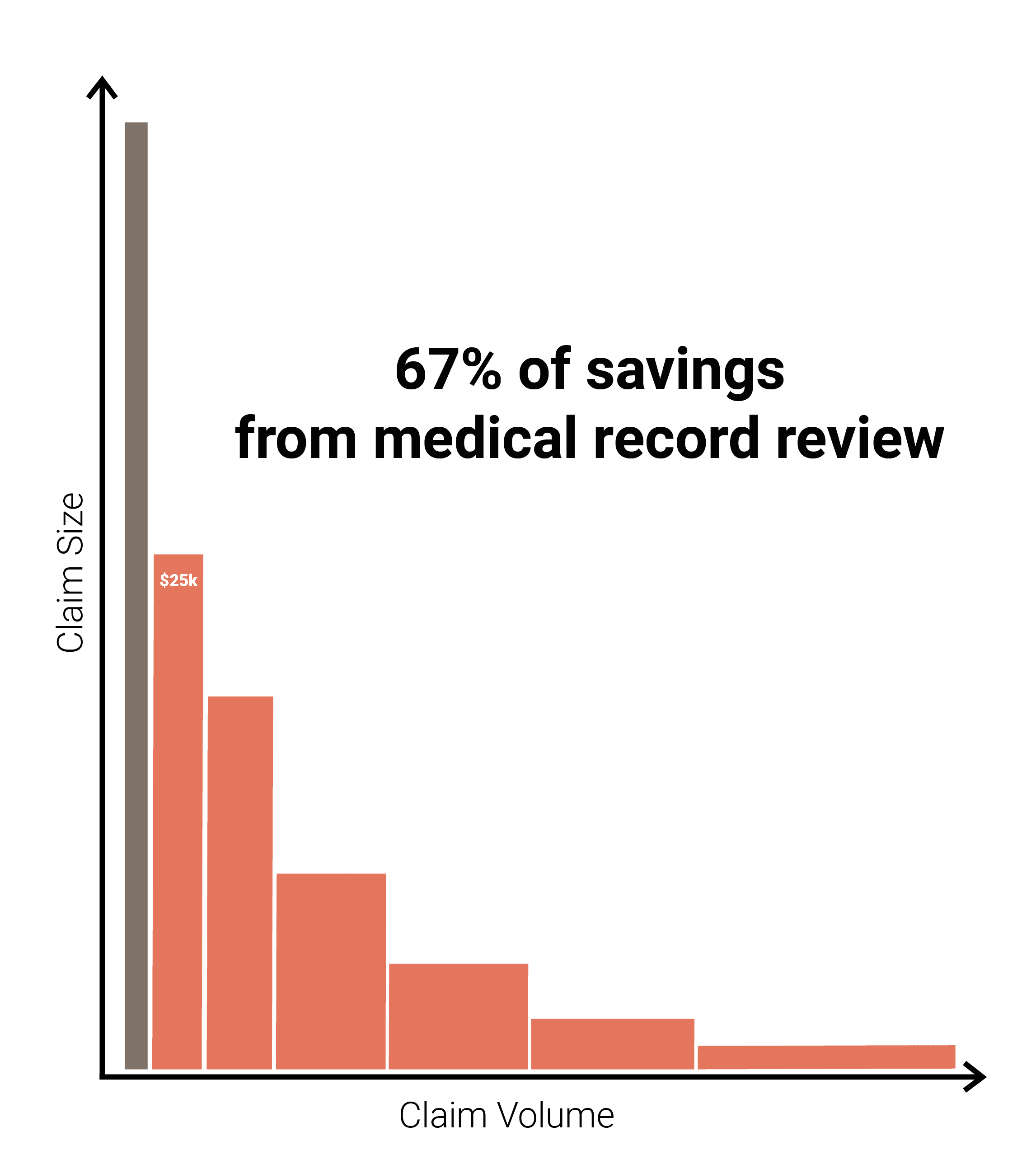
Other payment Integrity vendors have a floor below which they won’t perform any medical record review. That floor could range between $4,000 and $25,000.
Savings from medical reviews
At Nokomis, we generate approximately 52% of savings from reviewing medical records. So, wherever you set that bar, whether it be $4,000, $10,000 or $25,000, if you're not doing record review under that value, you're missing out on a significant amount of dollar savings.
At Nokomis, our team of in-house expert certified medical coders play a crucial role in the claim review process. Their extensive knowledge and experience allow us to identify errors in claims with unmatched accuracy and efficiency.
However, minimizing provider noise and abrasion is a key objective throughout our process. Being sensitive to providers is key and it is something we are proud of; just take a look at our appeal and denial overturn rates.
Appeal Rate
Our extremely efficient rules engine ClaimsWise™ and our highly experienced coding team allows us to achieve a 99.53% realization rate on every saving we identify.
We are not just about driving savings. We identify errors in a very complex and difficult claim submission and adjudication process.
We process all types of Claims
We are proficient in reviewing all professional and institutional claims, including the claim categories listed below. Our preference is to analyze all claims but we can slot into your existing vendor stack to focus on specific sets of claims.

Hospital inpatient
Hospital outpatient
Surgery center
Treatment center
Implants
We know that every client is different and believe in true partnerships.
So, we customize our service to fit your business profile and claims process; CMS, state legislation, rules, policies and contracts are all taken into account.
We customize the service specifically for you. We certainly don’t expect you to modify your processes to fit our process and our structure; we actually evolve and customize our product very heavily, so it fits within your business very succinctly.
We make it easy to do business with Nokomis which means:
Zero barrier to entry - no implementation cost
If we don’t save you money, we don’t take a fee
Rapid time to savings - a typical implementation is 8 weeks.
We work with national and regional plans, both fully insured and self-funded, with no client too large or too small.
We are big enough to deliver on our promise but small enough to really care.
The Nokomis service
is highly customizable
We can bypass edits for certain providers or members, and we can dial up or down the agressiveness of our rules. Our goal is to seamlessly operate and integrate with our clients’ business, and identify as many coding and billing errors as possible without causing undue strain on your organization or provider network.
We do our work and return all denial and reduction recommendations within one working day, which minimizes the impact on your payment timeline. And we view it like an ecosystem, a complex network of interconnected systems with interdependencies and symbiotic relationships, so maintaining this stability is paramount.
We have a highly customized system engineered to generate savings with negligible disruption. Remember those very low appeal and overturn rates. That creates a healthy environment, improving the overall health and performance of your healthcare ecosystem.
We run 100% of provided claims through ClaimWise™ every day.
Approximately 28% of claims trigger a code edit.
We request records on 8% of all claims that we review
Want to learn more? Let's talk.
Find answers to common questions about Nokomis' services, how they work, and the kind of results US Health Plans can expect.