What are the results and outcomes of Claim Accountability?
Payment integrity is an important part of the healthcare ecosystem. However, we’ve always believed in going beyond standard payment integrity. The healthcare claim submission process can be nuanced and complex, but it plays a vital role in outcomes for providers, payers, and patients alike. To amplify the impact of payment integrity, our team developed the Claim Accountability approach.
In short, Claim Accountability relies on both technology and human expertise to reduce inaccuracies and fraud in all healthcare claims, whether Medicare, Medicaid, or commercial insurance claims. This holistic approach gives our team a confident idea of what actually occurred in the exam room by requesting records for claims that have been identified for further review. With this more comprehensive approach, we’re able to find errors that payment integrity programs alone can often overlook. It’s a comprehensive claim review process that holds the healthcare system accountable.
But what impact does this approach have? What are the results or outcomes of Claim Accountability?
If you’ve been following along with our #ClaimOfTheWeek posts, you’ll know that Claim Accountability allows us to save an average of 5% to 13+%, even when the payor utilizes other payment integrity vendors prior to Nokomis’ review. But, did you know that:
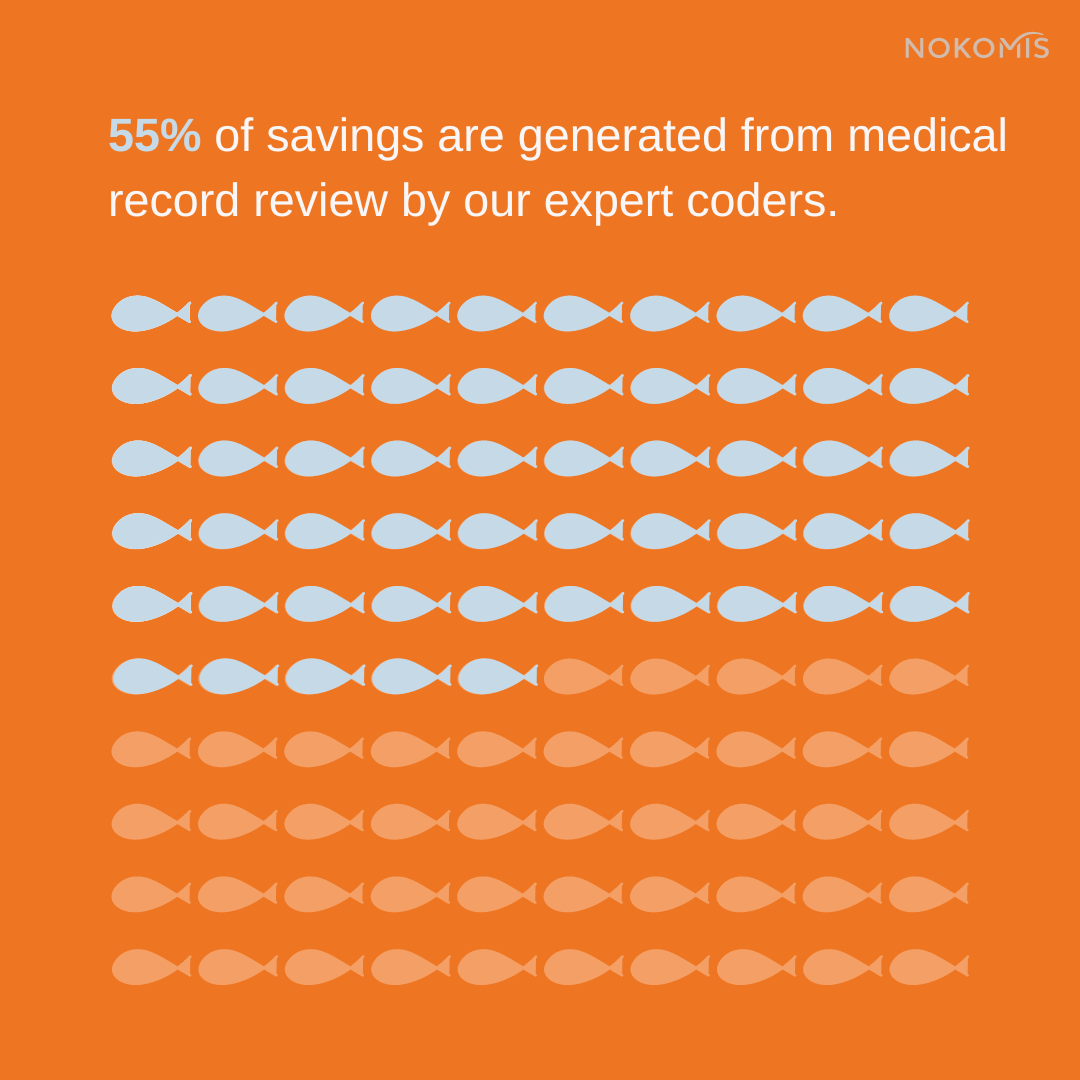
We combine our proprietary ClaimWise™ technology with a team of expert coders and analysts who have all worked on both provider and plan sides of healthcare. This holistic approach allows us to leverage the power and efficiency of technology, without losing human industry expertise.

We’re not in this as a “gotcha” game – we review claims with attention to detail and the intent to be as accurate as possible.
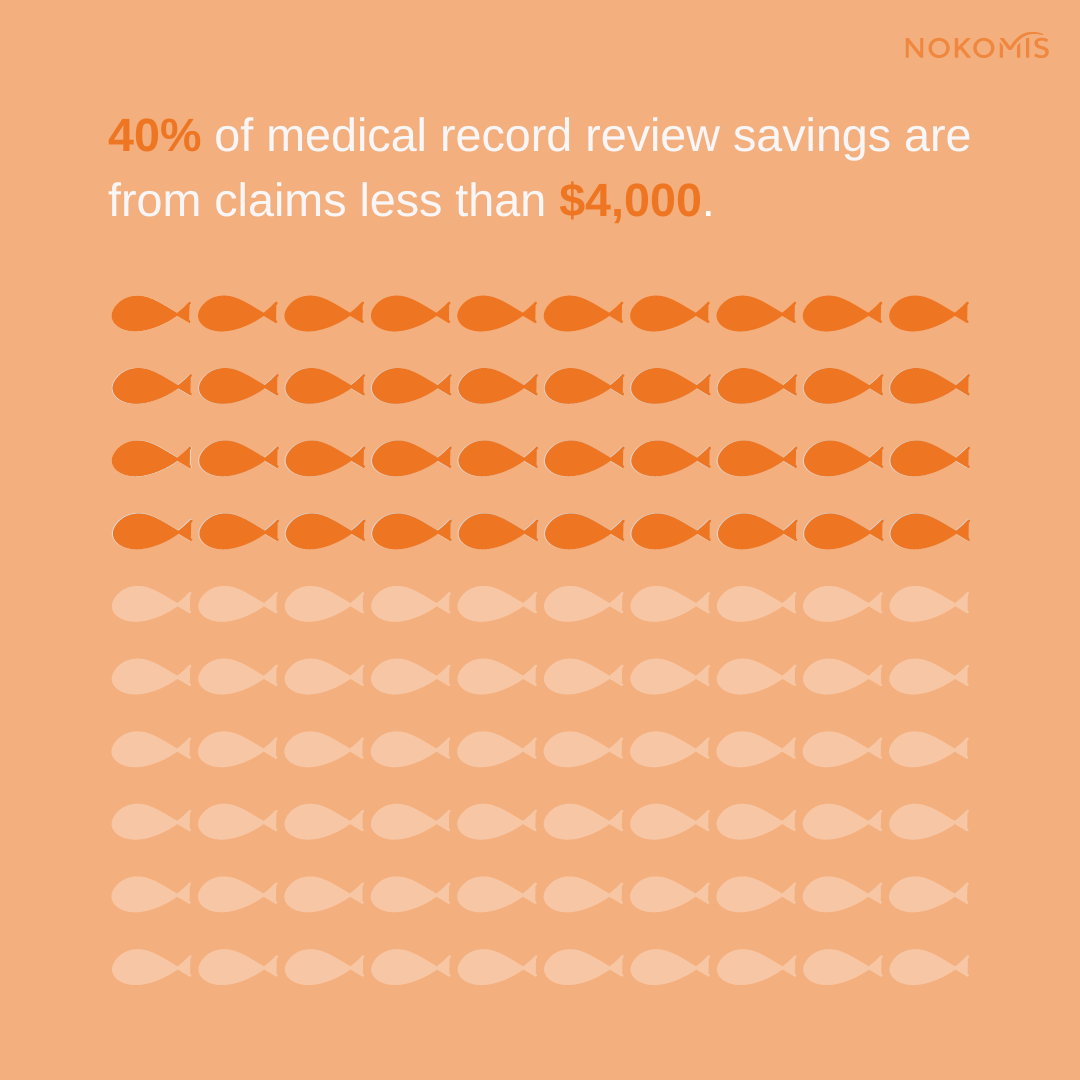
We review claims regardless of size. That means saving our clients thousands of dollars on some claims, and hundreds on others. Trust us, it all adds up in the end. We catch small dollar claim errors multiple times per day.
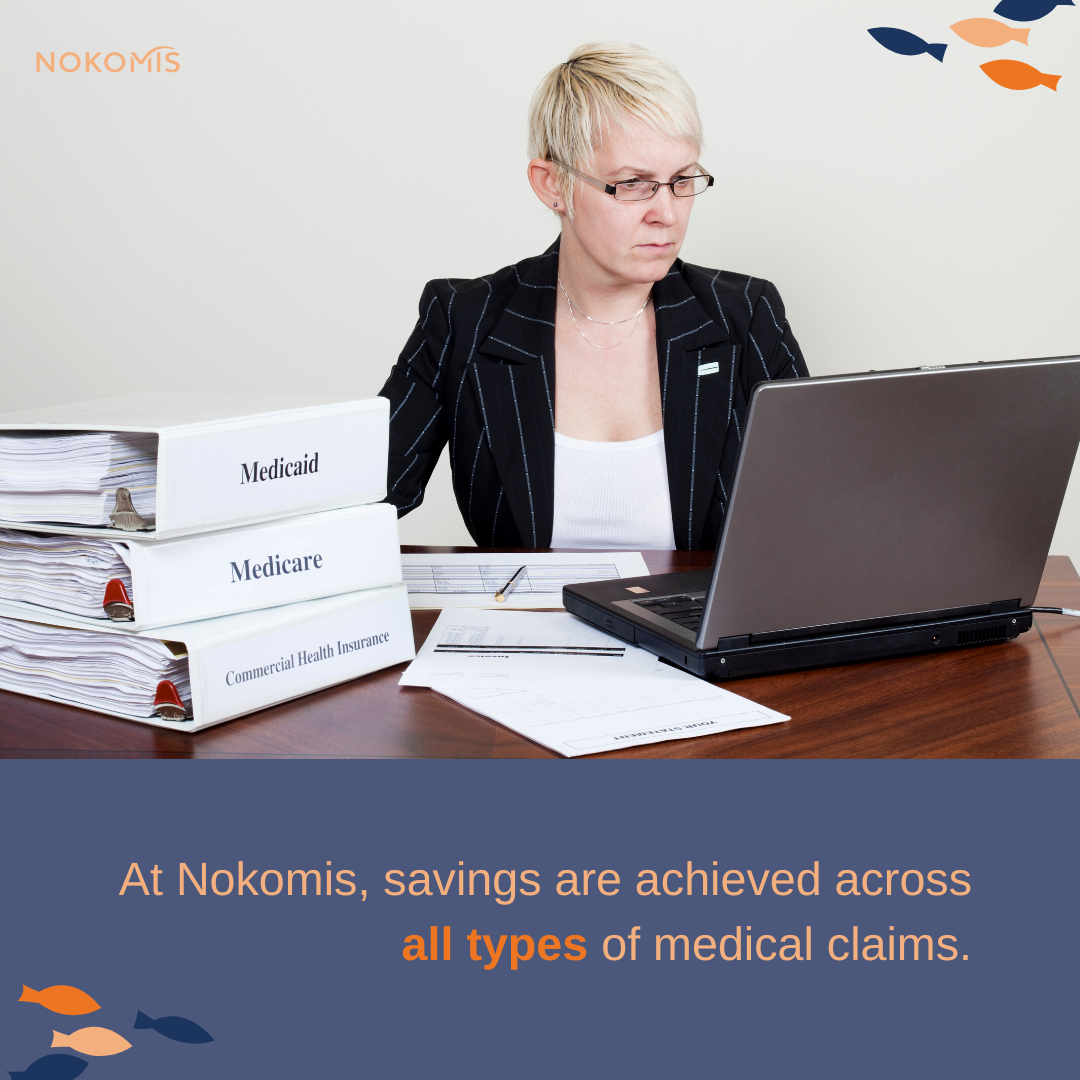
Just like we don’t cherry pick claims by size, we don’t only go for the heavy hitting claim types either. We review claims across all provider types and types of service.
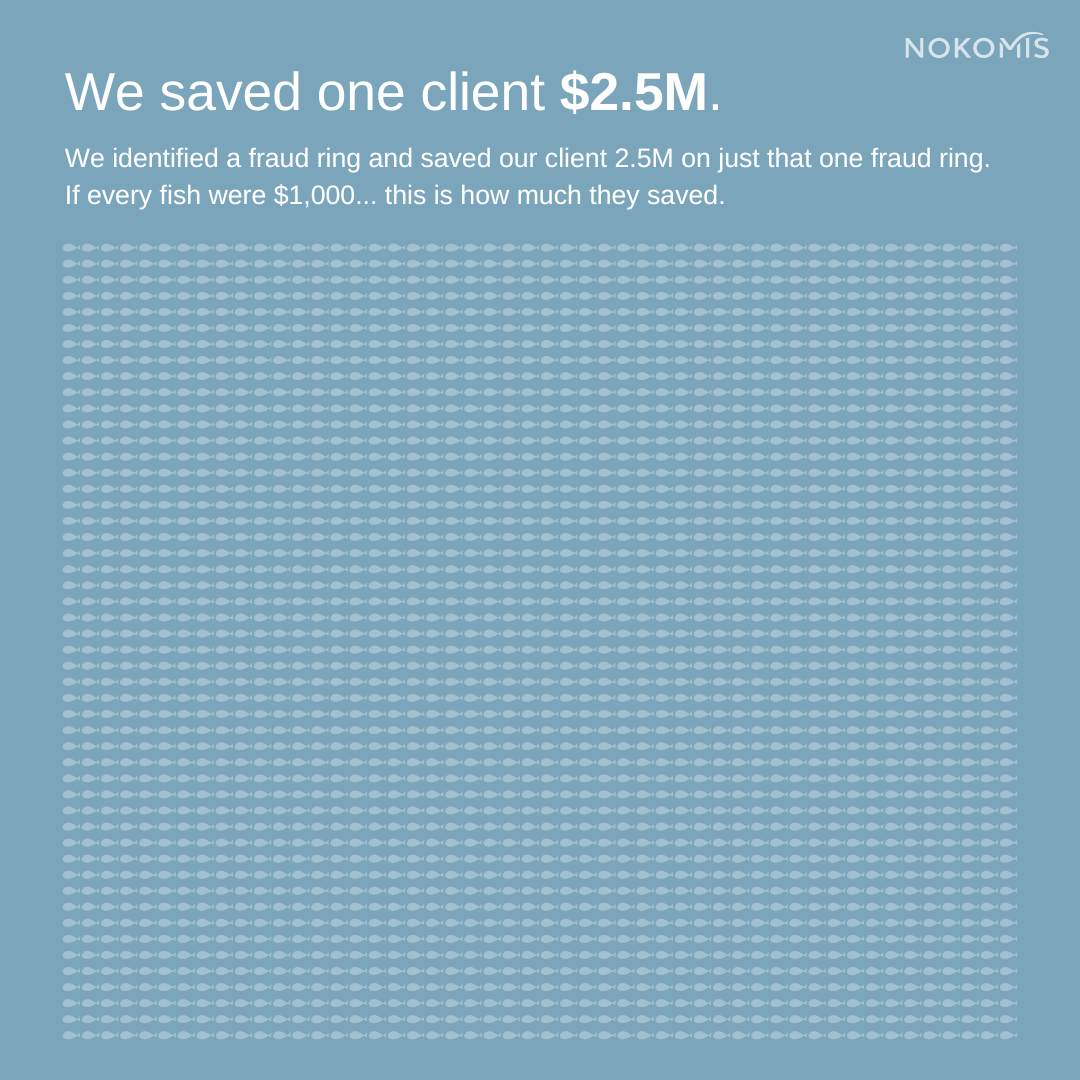
This one speaks for itself 😅
Interested in hearing more results from Claim Accountability? Contact us today!