What is Claim Accountability?

15 Apr 2022
How intelligent claim selection goes beyond payment integrity
When we think about medical coding from a patient’s perspective it can seem like an ironclad system: the doctor bills my health insurance for the services I received. Simple enough. However, what the average person isn’t seeing is the nuanced and complicated world of health claims coding. Let’s say a patient visits the emergency room after a fall and sustains a laceration of their knee. The provider (in this case, the emergency room staff), has to consider a number of things when billing for this incident, including the severity of the laceration, tests that the patient required, the policies of that patient’s health insurance, the rules and regulations of the hospital itself, and so on. With so many inputs, it can be challenging to submit an entirely accurate claim (especially as an overworked healthcare provider). Unfortunately, there’s also the opportunity for fraud in this system since health plans can really only know for sure what happened in the exam room by requesting records from the provider.
With all of that background in mind, it’s clear that medical billing is a complex and detailed process that requires expertise to navigate accurately.
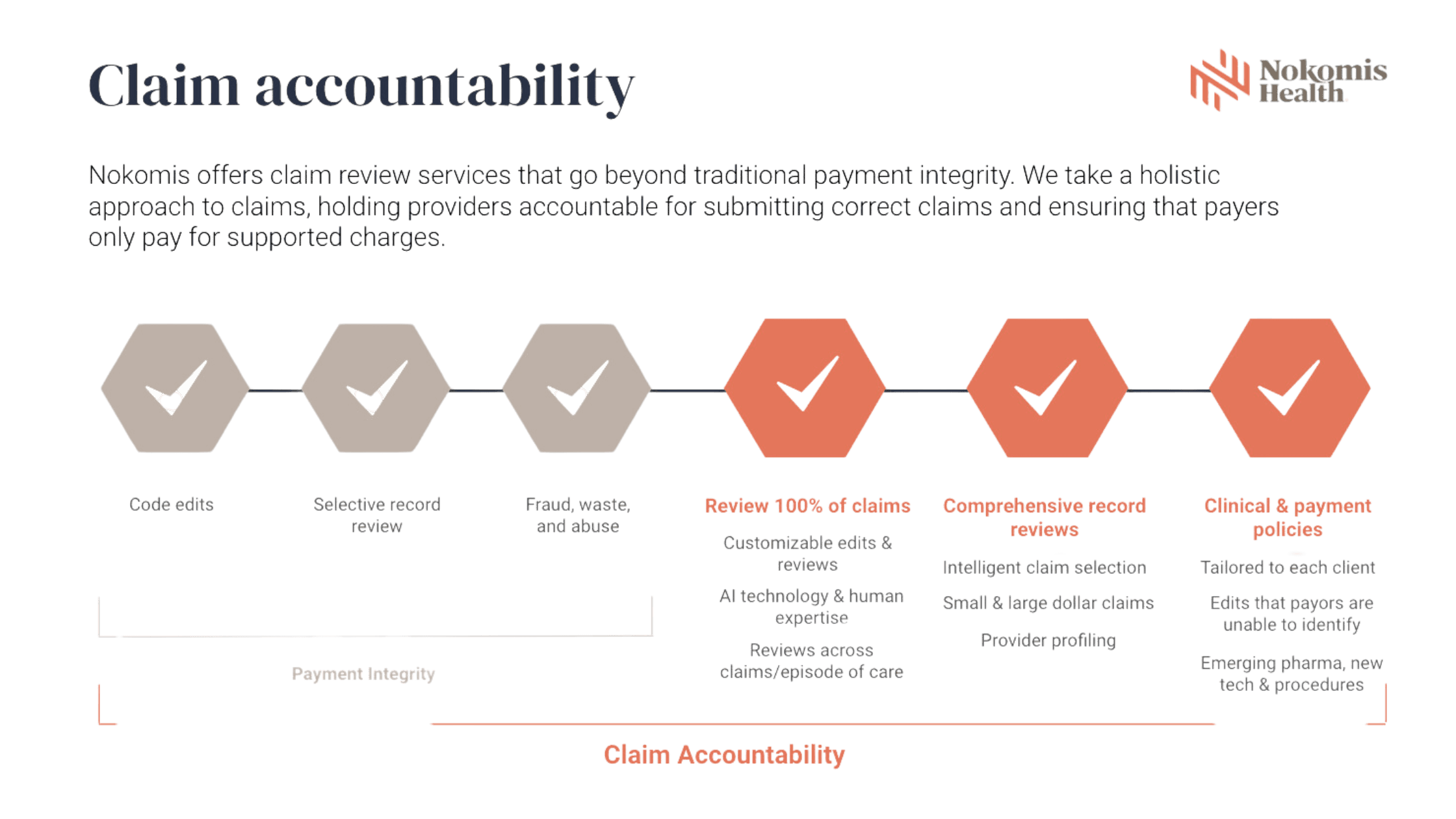
Up until recently, the main way that health plans ensured accuracy in the claims they paid was “payment integrity,” which is the process of reviewing a claim (usually with a technology-forward approach) to essentially scan the claim for inaccuracies and blatant fraud. A payment integrity approach works well for claims that look obviously inaccurate or suspicious, especially for large dollar claims. Payment integrity review often includes:
Code edits
Selective record review
Fraud, waste, and abuse
Now, where payment integrity can start to fall short is when you start talking about claims that look okay at face value (usually small dollar claims, ER claims, evaluation and management (E&M) fees, etc. …) but actually contain errors when given a more holistic review. These claims require a combination of human expertise and technology to effectively analyze, and require what we call “intelligent claim selection.” Together, intelligent claim selection and the combination of a human and technology review create what Nokomis has coined, “Claim Accountability.” Claim Accountability is a comprehensive claim review process that holds the healthcare system accountable. It includes an entire payment integrity review, plus:
Review of 100% of claims
Customizable edits & reviews
AI technology & human expertise
Reviews across claims/episode of care
Comprehensive record review
Intelligent claim selection
Small & large dollar claims
Provider profiling
Clinical and payment policies
Tailored to each client
Edits that payors are unable to identify
Emerging pharma, new tech & procedures
Claim Accountability was designed to reduce inaccuracies and fraud in all healthcare claims, whether Medicare, Medicaid, or commercial insurance claims. This holistic approach gives our team a confident idea of what actually occurred in the exam room by requesting records for claims that have been identified for further review. With this more comprehensive approach, we’re able to find errors that payment integrity systems alone can often overlook.
Now that we’ve established the “what” of claim accountability, let’s turn to the “how.” Claim Accountability is the combination of human expertise and innovation to find inaccuracies in all healthcare claims. We’re able to find inaccuracies that others overlook by leveraging our team’s expertise and judgment with the efficiency and intelligence of our technology. Diving deeper into human expertise, our team has decades of experience in claim review, most of them having worked with/for health plans and providers in the past. This extensive firsthand experience gives our team an acute eye for identifying claim inaccuracies, as well as locating claims that need further review. In tandem with our expert team, we use innovation to bolster our team’s efficiency. Our proprietary ClaimWise™ technology uses artificial intelligence to identify claim inaccuracies quickly, making it a highly specialized and unparalleled system for finding inaccuracies that other systems can miss.
In summary, Claim Accountability covers the same breadth as payment integrity, but then goes beyond existing standards to integrate intelligent claim selection, a review of 100% of claims, comprehensive record review, and clinical and payment policies, in addition to code edits, selective claim review, and fraud, waste, and abuse.